‘You will not touch my brain?!!’ said P; as I looked at the Magnetic Resonance Images of her Brain. There is a difference between ‘saying or instructing’ and ‘asking’; as in asking! ‘I might have to scratch the brain surface,’ I said.

Dr. Hillol Kanti Pal
Consultant Neurosurgery
Al Zahra Hospital -Dubai
I informed her that in my opinion her tumour was on the Brain surface and it should be possible to remove it using Stealth technology. Now there are two kinds of Stealth Technology. The first used by Putin’s latest Russian fighters evading radars in Ukraine and the Second is used by the Neurosurgeon to ‘get in and get out ‘with’ the Brain tumour’ without letting the Patient’s brain know that ‘Kilroy was here!’
‘But was P’s case doable by Stealth?’ was my thought. The technology resided only in my head and commissioning it would need Total Precision. Let me analyse the case for you:
1. 43-years old female, Severe raised intracranial tension for 48 hours
2. Investigated for a Right Upper Zone Lung lesion 4 months earlier. Inconclusive nature
3. One centimetre in front of Motor cortex and One centimetre medial to the Superior Sagittal Sinus. The ambush for the tumour had to be sprung between the Left Motor cortex and the Superior Sagittal Sinus. And she had preoperative right hemiparesis. That was good news for the neurosurgeon! Whether it would reverse following surgery is another question.
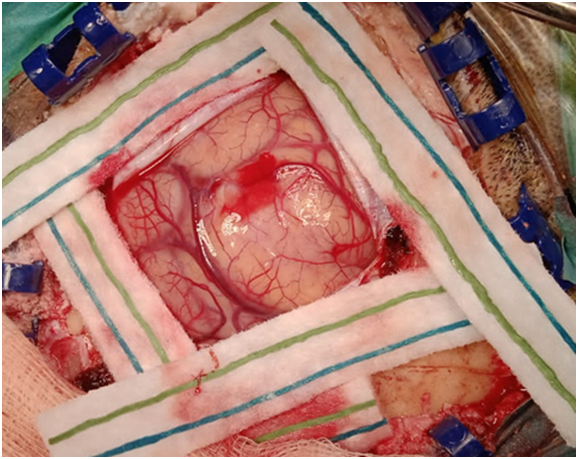
The Stealth coordinates in my Brain having been calculated, I had to land at the precise location which was the dome of the tumour, lock on to the tumour exposing it, use all resources I had to excise the tumour and escape undetected by P’s Brain – The Perfect ‘No-touch’ Technique.
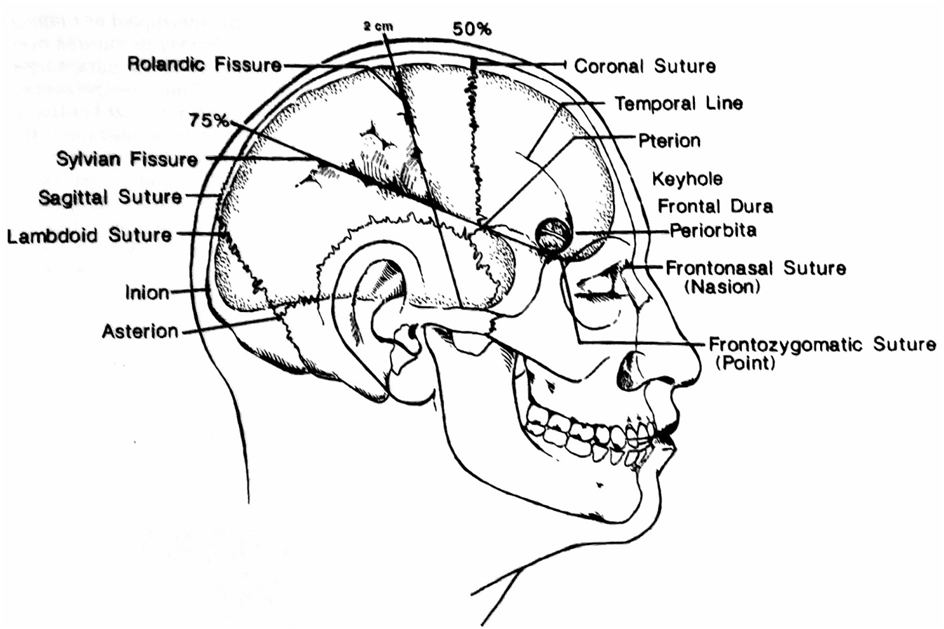
For decades we were taught as residents to mark out the eloquent areas of the brain. Like I said in this case it would be the Motor strip. I was fortunate that I could land on the chosen spot.

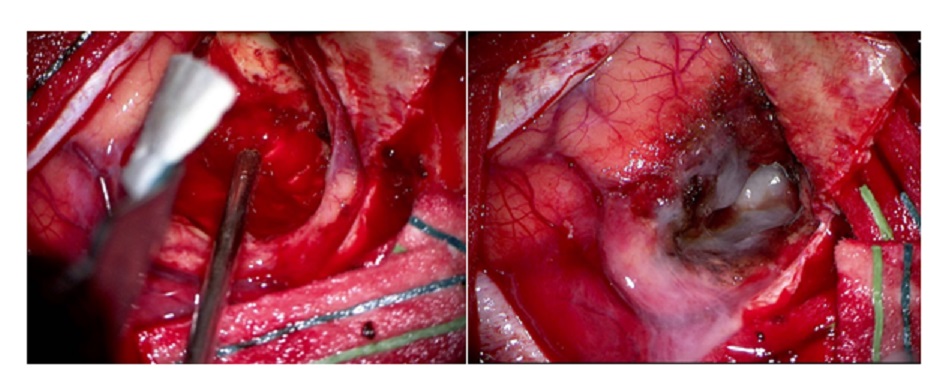
The gyrus overlying the tumour was obviously widened and broad. Aspiration yielded a haemorrhagic fluid. The tumour was encapsulated and could be delivered as a whole. But there was an area on the posterior superior aspect which was greyish red with sheaves of blood vessels coursing through it which still could be Glioma.
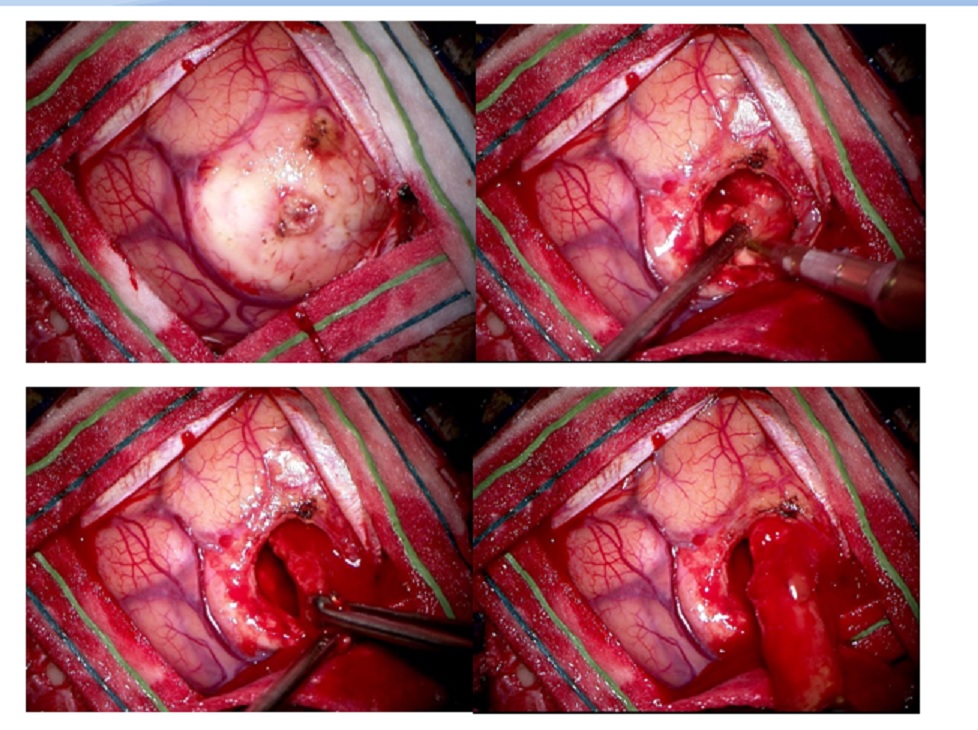
Dr. Houda provided excellent anaesthesia with a lax brain. I packed the tumour cavity with cotton balls to show that only the brain tumour was excised. Not a single millimetre of the normal cortex was touched. She recovered well and the right hemiparesis resolved within hours of surgery. Thanks to the ICU Team of Drs. Anas and Khamis; for close monitoring of the case preoperatively and postoperatively. These cases are tricky with a proclivity for sudden loss of consciousness due to hemorrhage in the Cystic tumour.
Her father-in-law had two surgeries for Hemorrhagic stroke which had left some scars. I reassured her husband that there would be no scar as the wound would be camouflaged as her hair regrows over the 50mm Craniotomy.
Dr. Hillol Kanti Pal
Consultant Neurosurgery